Integration & Automation (RPA)
Acrev solutions provides flexible and cost-effective billing services that cater to all your needs, empowering you to prioritize community service with undivided focus.
Integration Services
Acrev Solutions offers comprehensive Integration Services to seamlessly connect and integrate systems, applications, and data sources in healthcare. Our solutions streamline workflows, improve efficiency, and facilitate seamless information exchange. We specialize in


System Integration

Application Integration

HL7and API Integrations

Third Party Integration

Data Exchange and Interoperability

With Acrev Solutions Integration Services, you can achieve seamless data exchange, improved operational efficiency, and enhanced decision-making capabilities. Our team of experts combines technical expertise, industry knowledge, and a collaborative approach to deliver integration solutions that align with your organization's goals. Experience the benefits of streamlined workflows, accurate data exchange, and enhanced connectivity with Acrev Solutions' Integration Services.
Robotic Process Automation (RPA)
At Acrev Solutions, we offer cutting-edge Robotic Process Automation (RPA) services to revolutionize and streamline your healthcare operations. Our RPA solutions leverage advanced technology and intelligent automation to automate repetitive and rule-based tasks, enhancing efficiency, accuracy, and cost-effectiveness. Here's how our RPA services can benefit your organization:

Process Automation
Our RPA services enable the automation of manual, time-consuming processes within your healthcare operations. We identify areas of your workflow that can be automated and deploy RPA bots to handle these tasks. This frees up your staff's time and allows them to focus on higher-value activities, such as patient care and strategic decision-making.

Eligibility Verification
RPA bots can be utilized to automate the verification of patient insurance eligibility. By integrating with insurance portals and databases, the bots can retrieve real-time eligibility information, ensuring accurate billing and minimizing claim rejections or denials due to eligibility issues.

Payment Posting and Reconciliation
RPA streamlines the payment posting and reconciliation process by automating the matching of payment data with corresponding claims. Bots can quickly identify discrepancies, flag exceptions, and reconcile payments, reducing manual effort and improving accuracy.

Denial Management
RPA plays a vital role in denial management by automating the identification, analysis, and resolution of claim denials. Bots can systematically review denial codes, access relevant information, and initiate appropriate follow-up actions, such as resubmitting claims or appealing denials. This accelerates the resolution process and helps optimize revenue recovery.

Data Extraction and Reporting
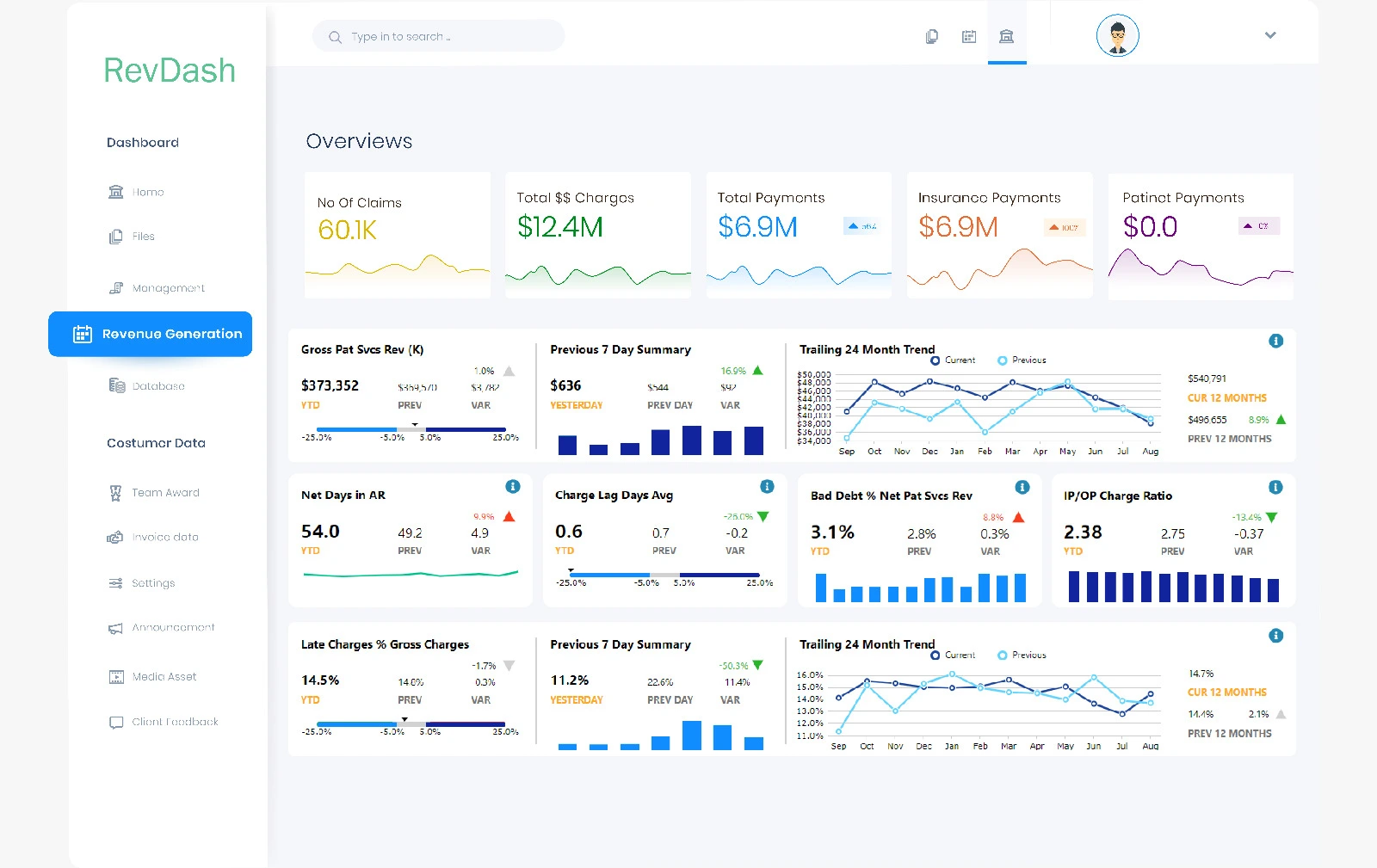
RPA can efficiently extract data from various sources and systems, consolidating information for reporting and analytics purposes. Bots can generate customized reports, providing valuable insights into key performance indicators, revenue trends, and operational efficiency, empowering informed decision-making and process improvement.

Scalability and Flexibility
RPA solutions offer scalability and flexibility, allowing you to adapt to changing business needs and handle fluctuations in workload. As your organization grows or undergoes process changes, RPA can seamlessly scale up or down to accommodate your requirements, ensuring consistent performance and efficiency.

Claims Processing
RPA can greatly enhance the efficiency of claims processing in medical billing. Our RPA bots can extract data from various sources, such as electronic health records (EHR) or scanned documents, and automatically populate the required fields in billing software. This reduces errors, accelerates the claims submission process, and improves reimbursement turnaround times.

Process Automation
Our RPA services enable the automation of manual, time-consuming processes within your healthcare operations. We identify areas of your workflow that can be automated and deploy RPA bots to handle these tasks. This frees up your staff's time and allows them to focus on higher-value activities, such as patient care and strategic decision-making.

Eligibility Verification
RPA bots can be utilized to automate the verification of patient insurance eligibility. By integrating with insurance portals and databases, the bots can retrieve real-time eligibility information, ensuring accurate billing and minimizing claim rejections or denials due to eligibility issues.

Payment Posting and Reconciliation
RPA streamlines the payment posting and reconciliation process by automating the matching of payment data with corresponding claims. Bots can quickly identify discrepancies, flag exceptions, and reconcile payments, reducing manual effort and improving accuracy.

Denial Management
RPA plays a vital role in denial management by automating the identification, analysis, and resolution of claim denials. Bots can systematically review denial codes, access relevant information, and initiate appropriate follow-up actions, such as resubmitting claims or appealing denials. This accelerates the resolution process and helps optimize revenue recovery.

Data Extraction and Reporting
RPA can efficiently extract data from various sources and systems, consolidating information for reporting and analytics purposes. Bots can generate customized reports, providing valuable insights into key performance indicators, revenue trends, and operational efficiency, empowering informed decision-making and process improvement.

Scalability and Flexibility
RPA solutions offer scalability and flexibility, allowing you to adapt to changing business needs and handle fluctuations in workload. As your organization grows or undergoes process changes, RPA can seamlessly scale up or down to accommodate your requirements, ensuring consistent performance and efficiency.

Claims Processing
RPA can greatly enhance the efficiency of claims processing in medical billing. Our RPA bots can extract data from various sources, such as electronic health records (EHR) or scanned documents, and automatically populate the required fields in billing software. This reduces errors, accelerates the claims submission process, and improves reimbursement turnaround times.
By leveraging Acrev Solutions' RPA services, you can transform your healthcare operations, streamline processes, and achieve greater productivity. Our team of experts works closely with you to understand your unique needs and design tailored RPA solutions to drive operational excellence. Embrace the power of RPA with Acrev Solutions and experience increased efficiency, accuracy, and cost savings in your healthcare organization.
Acrev Solutions Empowers You to
Achieve Financial Resilience by Engaging our
Revenue Cycle Management (RCM) Experts.